Are you ready for ICD-10?
What is ICD?
The International Classification of Diseases (ICD) is the standard diagnostic tool for epidemiology, health management and clinical purposes. ICD is used by physicians, nurses, other providers, researchers, health information managers and coders, health information technology workers, policy-makers, insurers and patient organizations to classify diseases and other health problems. ICD, published by the World Health Organization (WHO), includes unique alphanumeric codes to identify known diseases and other health problems, and is used to monitor the incidence and prevalence of diseases and other health problems, providing a picture of the general health situation of countries and populations.
Why the transition to ICD-10?
The ICD-9 to ICD-10 transition updates diagnosis coding and better reflects current medical diagnoses, practices, techniques, and technology. With the diagnosis coding transition, 13,000 ICD-9 codes will be expanded to 68,000 ICD-10-CM codes, allowing healthcare providers to better define a patient’s diagnosis, especially in conjunction with electronic health records (EHRs).
What are the benefits of ICD-10?
The move to ICD-10 is expected to streamline the process that healthcare providers use to submit medical claims. The streamlining will result in fewer coding mistakes, less need for supporting documentation and as a result, fewer requests for additional information after a claim has been submitted. Other benefits, according to the Centers for Medicare & Medicaid Services, include better sensitivity in refining grouping and reimbursement methods, and improvements to public health surveillance.
Due to the increased specificity of the ICD-10 codes, it will require higher-quality and more detailed clinical documentation which will provide a more accurate clinical picture of the quality of care provided.
In general, ICD-10 will allow healthcare providers to do the following:
- Improve quality measurement
- Reduce errors in diagnosis coding
- Improve analysis of disease patterns
- Improve tracking and response to public health issues and outbreaks
- Incorporate greater specificity and clinical information
- Decrease the need to include supporting documentation with claims
- Increase sensitivity for grouping and reimbursement methodologies
- Improve the efficiency of claim submissions, especially with EHR and Practice Management Software
What is effective date of ICD-10?
The ICD-9 code sets used to report medical diagnoses and inpatient procedures will be replaced by ICD-10 code sets on October 1, 2015. ICD-10 consists of two parts:
- ICD-10-CM diagnosis coding which is for use in all U.S. health care settings.
- ICD-10-PCS inpatient procedure coding which is for use in U.S. hospital settings.
Determination of which code set to use is driven by the date of service and not the billing date. For outpatient and physicians claims, the date of service dictates which code set to use, while the date of discharge dictates which code set to use for hospital inpatient claims.
- Claims for services provided on or after October 1, 2015 must be coded in ICD-10
- Claims for services provided prior to October 1, 2015 must be coded in ICD-9
- No claim can contain both ICD-9 and ICD-10 codes
- Any claim for dates of service on or after October 1, 2015 that contains ICD-9 codes will be rejected
What is the ICD-10 code structure?
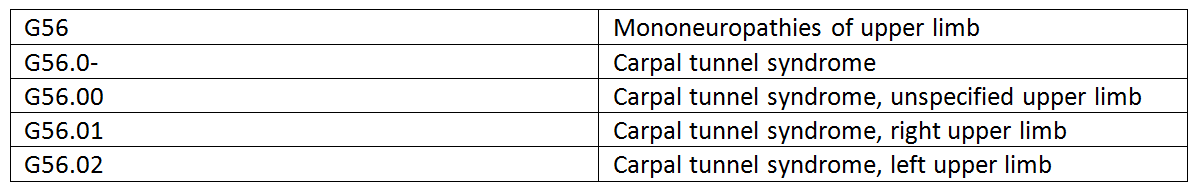
ICD-10 diagnosis codes have between 3 and 7 characters. Codes with three characters are included in ICD-10-CM as the heading of a category of codes that may be further subdivided by the use of any or all of the 4th, 5th, and 6th characters. Digits 4-6 provide greater detail of etiology, anatomical site, and severity. A code using only the first three digits is to be used only if it is not further subdivided.
A code is invalid if it has not been coded to the full number of characters required. This does not mean that all ICD-10 codes must have 7 characters. The 7th character is only used in certain chapters to provide data about the characteristic of the encounter.
1st character – is alpha
2nd and 3rd characters – are numeric
4th to 7th characters – are alpha or numeric
Example: G56 – Mononeuropathies of upper limb
Who is affected by the ICD-10 diagnosis codes?
Everyone working in the U.S. health care system will be affected by the industry’s transition to ICD-10 diagnosis codes. This is a major change requiring time, effort and preparation, and anyone who uses medical diagnosis codes, and is covered by the Health Insurance Portability Accountability Act (HIPAA), will be impacted such as:
- Physicians and other health care providers
- Health insurance companies (payers)
- Clearinghouses
- Third party billing services
- Software vendors
How does AAFCPAs advise you to prepare for ICD-10?
The transition is now under a month away. AAFCPAs advises clients to act now to avoid rejection of claims. It is not too late to ensure that you are adequately prepared.
AAFCPAs has provided the following brief list of action items that you may address over the next few weeks to ensure timely compliance:
- Identify when and where ICD-9 codes are currently being used in your practice. Ask all staff members for their input. These are the areas that will be affected the most by the transition.
- Talk to your vendors (Electronic Medical Records & Practice Management System) to ensure their compliance with the new ICD-10 code set. Are their systems ready to accommodate the ICD-10 codes?
- If you outsource your billing, be certain your service provider is upgrading their systems.
- Assess staff training needs and develop programs to support both the initial and any ongoing training.
- Check with your payers about their systems upgrades and results of their testing.
- Review your payer contracts and determine whether new ones will be required.
- Evaluate all systems and potentially revise work flows/processes if necessary.
- Manage expectations regarding productivity loss during initial implementation phase.
The healthcare industry has more changes to come. ICD is again under revision, subject to an ongoing revision process, and the WHO has announced the release date for ICD-11 is 2018.
If you have any questions about creating/revising, or adding efficiency to your ICD-10 coding processes, please contact your AAFCPA partner, or Matt Hutt at 774.512.4043, mhutt@nullaafcpa.com.

